Pelvic Fracture Treatment In Elderly
Pelvic fractures in older persons create significant medical problems that frequently result in prolonged hospital stays and diminished movement abilities together with elevated complication threats.
The growing numbers of older adults require complete knowledge about treatments for pelvic fractures because they need rehabilitation strategies for these injuries. The article examines causes and treatment methods and recovery strategies for pelvic fractures among elderly people along with statistical observations.
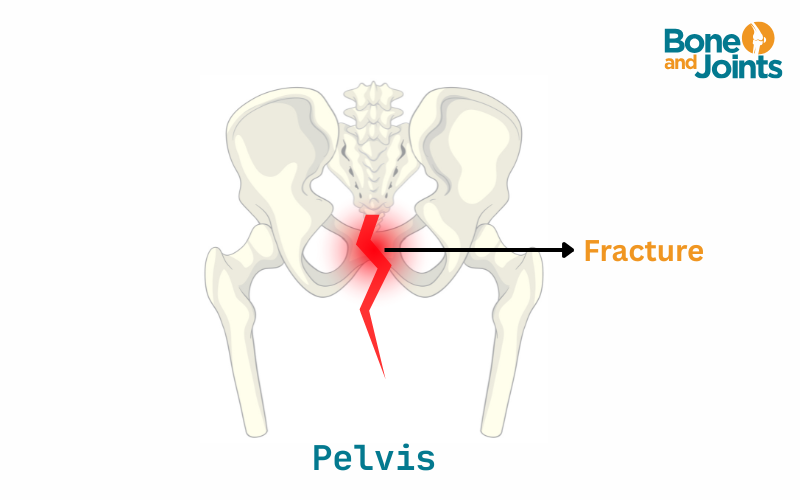
Understanding Pelvic Fracture In Elderly
The Medical Field Requires Knowledge about Pelvic Fractures that Affect Elderly Patients.Generally pelvic fractures in mature individuals result from minimal-energy incidents like sliding on wet surfaces or collapsing when standing. Senior patients with osteoporosis have weaker bones than younger people which makes them susceptible to pelvic fractures when experiencing even simple falls.
A combination of different risk elements leads to pelvic fractures in older adults. The aging condition called Osteoporosis ranks as one of the most important health problems since it impacts around 44 million Americans older than fifty. Seniors experience higher falls risk from their poor muscle strength along with their difficulty keeping balance and the dizziness and coordination problems associated with particular medications. Pearson's disease severity affected by arthritis and neurological conditions leads to stability weakening which results in increased risks for elderly people during pelvic fractures.
Read: How To Deal With Pelvic Pain When Sleeping At Night?
Types of Pelvic Fractures in Seniors
The pelvic fractures that affect elderly individuals fall into three principal categories.
-
Stable fractures: Stable fractures of the pelvic bones present with tiny yet generally healable cracks that can be treated with basic care.
-
Unstable Fractures: Medical professionals classify these fractures as unstable because multiple pelvic bones break frequently necessitating surgical intervention because of severe misalignment.
-
Acetabular fractures: This is the fracture in the hips and includes hip replacement surgery when severe joint damage occurs in patients.
Treatment Approaches for Pelvic Fractures in the Elderly
There are many ways to effectively isolate and get the patient relieved from pelvic Fractures. Let’s discuss those in detail:
1. Emergency Care and Pain Management
Older patients who experience pelvic fractures face a serious danger of internal bleeding along with deep vein thrombosis (DVT) and organ injury. Stabilization of affected patients with concurrent pain control stands as the immediate primary goal of medical assistance. Emergency medical staff begin by performing vascular tests and CT scans along with MRI imaging followed by intravenous fluids and blood transfusions to treat the fracture injury.
Sufferers receive prompt pain control as a key treatment priority during the first stage of care. For treatment of intensive pain conditions health professionals either use opioids or they select acetaminophen and nerve-blocking methods when caring for elderly patients to reduce side effects such as confusion and sedation.
2. Non-Surgical Treatment
The majority of pelvic fractures among elderly patients (70%) do not require surgical intervention because they maintain stable fracture status. Treatment of pelvic fractures in elderly patients includes three main elements which are bed rest along with pain management and physical therapy.
Both medical professionals and patients need to balance bone healing with the risk of complications since short-term bed rest is necessary but long-term immobilization should be avoided. Medical professionals recommend assistive devices including walkers or crutches because they enable patients to rebuild their ability to move.
The early introduction of physical therapy through treatment prevents patients from losing their physical condition. The implementation of gentle exercises that move joints allows patients to protect both muscles and joints from forming blood clots during recovery.
3. Surgical Intervention
Medical doctors commonly perform procedures on unstable pelvic bones to fix the stability and restore movement capabilities. The need for surgery arises from pelvic fractures that both limit walking ability and produce severe pelvic bone misalignment and life-threatening bleeding into the body.
The treatments for pelvic fractures usually involve these procedures:
-
External Fixation: The treatment method of External Fixation uses external metal rods together with screws which hold pelvic bones stable.
-
Open Reduction and Internal Fixation(ORIF): Medical staff perform Open Reduction and Internal Fixation (ORIF) by inserting metal plates along with screws during surgical procedures to straighten and secure broken bones in position.
-
Hip Replacement: A hip replacement surgery is suitable for patients whose hip socket (acetabulum) suffers severe damage beyond effective repair.
Elderly patients undergoing surgery for pelvic fractures experience elevated risks of infections and deep vein thrombosis and post-surgical delirium besides surgical success in restoring mobility. Research findings demonstrate that patients who undergo suitable surgical treatment during the early stages achieve better mobility recovery results in the long run.
Rehabilitation and Recovery
Rehabilitation and recovery phases are often guided by strong changes in lifestyle factors. The following things must be thoroughly considered
1. Physical Therapy and Early Mobilization
The success rate of pelvic fracture recovery depends on getting patients out of bed early for treatment and rehabilitation. A research study in the Journal of the American Geriatrics Society revealed that geriatric patients who initiate physical therapy soon after their pelvic fracture experience thirty percent better results in becoming mobile independently relative to patients who stay inactive.
The main aspects of physical therapy for pelvic fracture patients target core muscle growth along with training of pelvic floor muscles while simultaneously working on balance and walking progress. Such physical exercises serve two functions: they help recovery progress and decrease the possibility of new falls.
2. Fall Prevention Strategies
The risk of another fall occurs in thirty percent of elderly people who experience pelvic fractures meaning fall prevention stands as an essential aspect of their recovery care. Medical professionals must adopt preventative measures including hazard clearance, bathroom barrier installation and home lighting enhancement to decrease subsequent fall occurrences.
The management of osteoporosis remains important because it decreases the chances of secondary fractures. Physicians prescribe both calcium supplements with vitamin D supplements along with drugs that boost bone strength. Physical exercise that requires body weight as resistance supports both bone strength and stable body positioning.
3. Psychological and Emotional Well-being
Elderly patients suffer significant psychological effects when they get pelvic fractures. Depression and anxiety combined with a fear of re-falling among patients result in diminished confidence regarding their independence when walking. The recovery mindset of elderly patients can be supported by emotional vitality which requires counseling and caregiver motivation along with social networking.
Learn More: Can You Increase Your Bone Density After 70?
Prognosis and Long-Term Outcomes
Research shows that elderly people who suffer pelvic fractures experience a mortality rate of 10-20% throughout their first year because of infections along with immobility complications and existing health problems. Nevertheless patients who receive timely medical care and complete rehabilitation help them reach more than 60% improvement in their independence.
Complete healing occurs during six to twelve weeks for mild fractures yet healing after severe fractures that need surgery extends to six months. The improvement of long-term results requires ongoing physical therapy sessions combined with lifestyle adaptation approaches.
Conclusion
A multidisciplinary method is needed to treat pelvic fractures in elderly patients because it integrates medical approaches with rehabilitation and fall prevention techniques to achieve optimum recovery outcomes. The path of recovery becomes successful when patients receive clinical interventions and start moving following their fractures based on their condition's seriousness. Elderly patients who receive total care services will build independence while decreasing the chances of more fractures in the future.